A groundbreaking advancement in the treatment of Type 1 diabetes has been achieved through the collaboration of scientists from Cornell University and the University of Alberta. They have developed an implantable device, known as SHEATH (Subcutaneous Host-Enabled Alginate THread), offering a promising alternative to the traditional insulin injections or pumps currently used in managing this chronic condition.
A Leap in Diabetic Care
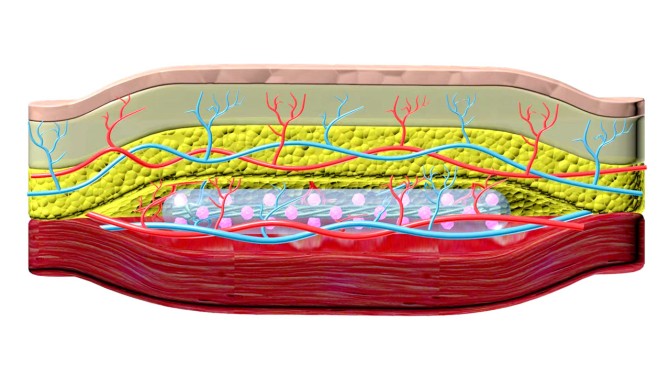
The SHEATH device is designed to secrete insulin via islet cells, which are naturally responsible for insulin production in the body. This thread-like implant is placed under the skin in a two-step process. Initially, nylon catheters are inserted subcutaneously, around which blood vessels form, providing structural support for the islet devices that are later placed in the created space. These islet devices, measuring about 10 centimeters in length, not only secrete insulin but also receive vital nutrients and oxygen from the surrounding blood vessels.
The Evolution of SHEATH
The journey to SHEATH began with the development of TRAFFIC (Thread-Reinforced Alginate Fiber For Islets enCapsulation) in 2017 by Cornell’s Minglin Ma. This earlier version of the implant was designed to be placed in the patient’s abdomen. In 2021, a more robust device was created, demonstrating the ability to control blood sugar levels in mice for six months. The current version, SHEATH, marks a significant advancement in this line of research, combining innovative strategies to improve cell survival without the need for immunosuppression.
Overcoming Clinical Challenges
While the potential of SHEATH is immense, challenges in its long-term application remain. The primary concern is maintaining the functionality of the islets for extended periods within the body. Researchers are exploring ways to maximize nutrient and oxygen exchange in large-animal models and eventually in patients. The hope is that future iterations of the device could last from two to five years before needing replacement.
A Collaborative Triumph
The collaboration between Cornell and the University of Alberta has been pivotal in this development. James Shapiro of the University of Alberta, a renowned figure in islet transplantation, contributed significantly to this project. The collaboration successfully merged their respective innovative approaches to create a system that avoids the need for immunosuppression while effectively managing Type 1 diabetes.
Clinical Implications and Future Prospects
The SHEATH system has shown promising results in diabetic mice, reversing the condition without necessitating immunosuppression. The system has also been tested successfully in minipigs, showcasing its scalability. Despite the hurdles in clinical utility, the team remains optimistic about the device’s potential impact on diabetic care.
The research, supported by various health and diabetes research foundations, represents a significant stride towards a less invasive, long-term solution for Type 1 diabetes management. This innovation paves the way for a future where daily insulin injections could become a thing of the past for millions affected by this disease.